Acupuncture Mechanism Studied By MRI
Evidence from Neuroimaging Studies
Evidence from Neuroimaging Studies: How Acupuncture Affects Brain Activity
Recent advancements in neuroimaging have helped clarify how acupuncture points correlate with the functions they are believed to influence. Dr. Zhang-hee Cho, a professor at UC Irvine’s Department of Radiological Sciences, pioneered this research, demonstrating that acupuncture at specific points affects brain activity.
Dr. Cho’s Groundbreaking Study
In 1998, Dr. Cho and his colleagues published a study in the Proceedings of the National Academy of Sciences, showing that needling acupoints near the little toe for eye-related issues activated the visual cortex in a group of 12 volunteers. This result suggests that acupuncture can stimulate specific brain areas linked to the corresponding body functions.
In contrast, when Dr. Cho stimulated nearby points, just a few centimeters away from the original acupoints, no activation in the visual cortex occurred. This finding indicates that acupuncture’s effects are precise, targeting specific areas of the brain based on the points being stimulated.
Dr. Gollub’s Research on Real vs. Sham Acupoints
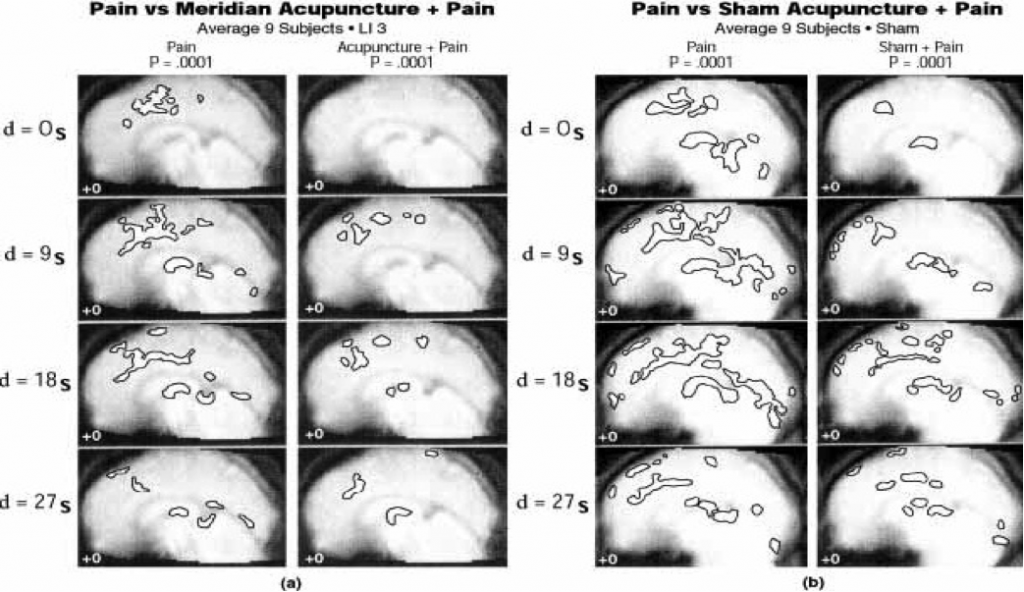
Dr. Randy Gollub, Assistant Director of Psychiatric Neuro-Imaging at Massachusetts General Hospital, is investigating the differences in brain activity when real acupoints are needled versus sham (fake) points. Early results suggest that both types of acupuncture activate similar regions of the brain responsible for pain management, with a stronger response seen for true acupoints.
Dr. Gollub compares the acupuncture points to mountain peaks, stating that even if the needle is placed in a “valley” (a non-optimal location), acupuncture still has an effect. The key takeaway is that acupuncture treatments—whether at real or sham points—appear to trigger biochemical responses in the brain, promoting pain relief and overall well-being.
Acupuncture and Biochemical Messages
Dr. Cho’s research suggests that acupuncture triggers biochemical messages between the brain’s hypothalamus and the pituitary and adrenal glands. These messages influence the body’s response to stressors such as pain, emotional trauma, or infection, by adjusting the production of certain stress hormones. This mechanism may explain why acupuncture can provide lasting pain relief and help manage various health conditions.
Dr. Cho also predicts that future acupuncture treatments may involve fewer needles, as a single well-placed needle could provide the same or even better results for pain relief, streamlining the treatment process.
Gate-Control Theory of Pain and Acupuncture
The Gate-Control Theory of Pain, developed independently of acupuncture in neuroscience, posits that pain perception is modulated by a balance between excitation and inhibition of pain pathways. This theory suggests that pain can be “gated” or blocked through various physiological, psychological, or pharmacological mechanisms.
Acupuncture is believed to activate this central control of pain at the brain level, rather than at the spinal cord or peripheral areas, through the release of endogenous opioid neurohormones such as endorphins and enkephalins—the body’s natural painkillers. These neurohormones help manage pain by altering the perception of discomfort at the brainstem reticular formation.